FINALS
Section A (point, draw, explain)
1. Virus
2. Immune response
3. Tolerance
4. Immunodeficiency
5. B cells humoral immunity
6. Vaccine
7. Hypersensitivity
8. Agglutination
Section B
1. GVHD
2. Immune response to tumor cells/cancer cells
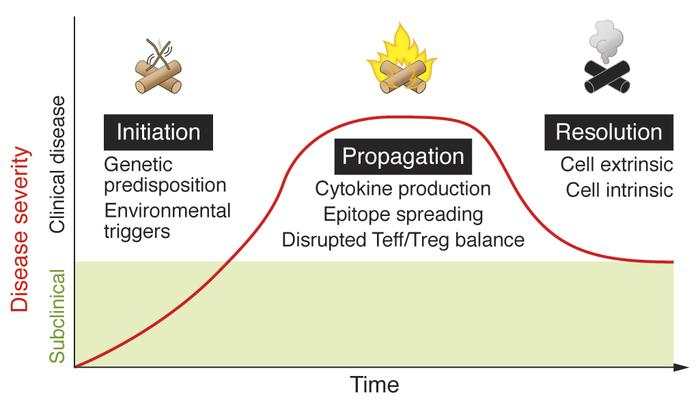
3. Autoimmune
4. Immunoproliferative disorder
November 2020
SECTION A: SHORT ANSWER QUESTIONS (60 MARKS)
1. Regarding primary immunodeficiency (PID):
a. Describe the characteristics of ONE (1) humoral immunodeficiency type that occurs during adulthood (20-40 years old). (7 Marks)
Common variable immunodeficiency
- defects in B cell differentiation into plasma cells
- complications: autoimmune disorder, lymphoid malignancy, bronchiectasis to recurrent pulmonary infections
- diagnosis: peripheral lymphadenopathy, family history, H/O recurrent infections
- lab: low IgG, IgA, IgM, antibody titer (against DPT/MMR vaccines)
- treatment: IVIG, immunosuppressant, antibiotics (chronic lung infections)
https://www.msdmanuals.com/professional/multimedia/table/humoral-immunity-deficiencies
b. Name THREE (3) types of X-linked related PIDs. (3 Marks)
X linked agammaglobulinemia
Wiskott Aldrich syndrome
Hyper IgM syndrome
2. Name TWO (2) major systemic autoimmune diseases and describe the disease characteristics of each. (10 Marks)
SLE
- chronic
- risk factor: genetic defects, UV radiation, smoking, infection, medication
- complication: cardiovascular disease, serious infections, renal failure, hypertension, antiphospholipid syndrome
- signs and symptoms: fever, joint pain, rash, weight loss
- diagnosis: malar rash, discoid rash, arthritic >2 joints, serositis, oral/nasal ulcers, neuro/renal/hematological disorder, photosensitivity
Rheumatoid arthritis
- chronic
- risk factors: genetic predisposition, smoking
- complications: pericarditis, anemia, carpel tunnel syndrome
- signs and symptoms: inflammatory polyarthritis, morning stiffness, malformation (ulnar deviation)
- x ray: soft tissue swelling, low bone density, narrow joint space
- lab: normocytic anemia, high rheumatoid factor titer, high ESR & CRP
3. Provide examples of the innate and adaptive immune components that play roles in tumor surveillance. (10 Marks)
4. Compare between hyperacute, acute and chronic graft rejection based on their onset, mechanism, and the type of hypersensitivity involved. (10 Marks)
5. Describe the immune defects associated with HIV-1 infection on B-cells and CD8 T cells. (10 Marks)
6. Briefly explain FIVE (5) types of vaccine. (10 Marks)
Live attenuated vaccines
- often consists of a pathogenic strains in which the virulent genes are deleted or modified
- weakened pathogen (still can replicate)
- more effective than a killed or subunit vaccines
- TB-BCG contains a live attenuated strain of bovine strain of TB (Mycobacterium bovis)
- measles, mumps, rubella, yellow fever
- advantage:
- single, small dose
- natural route
- local and systemic immunity
- resembles natural infection
- disadvantage:
- contaminating virus
- reversion to virulence
- inactivation by climate changes
- risk factors:
- microbe with immunosuppressive agents
- attenuated strains with residual virulence due to incomplete inactivation
- attenuated strains can recover their virulence in other hosts after released into environment
Inactivated vaccine
- contains copies of virus that have been killed or inactivated (use heat or formalin)
- not effective as live vaccines but safer
- Polio, rabies, HAV, influenza
- cholera, pertussis, typhoid
- advantage: no reversion to virulence, more stable, easier storage and transport
- disadvantage: high or multiple doses (cause allergy), incorporation of adjuvants (increase inflammation)
Toxoid vaccine
- contains purified and inactivated toxins (use formalin)
- often combined with subunit vaccine
- Diphtheria, tetanus, pertussis
- advantage: highly immunogenic, safe, sterile
- disadvantage: possible contamination by toxins, call for adjuvant, cause allergy/infiltration at injection site
DNA vaccine
- contain DNA codes for specific proteins (antigens) from a pathogen
- injected into cells
- proteins processed by host cells and displayed on surface
- recognize proteins as foreign
- trigger immune responses
- synthesize proteins
- advantage:
- induction of long term immune response
- induction of both humoral and cellular
- possibility of contructing multiple epitopes in plasmids
- heat stable
- ease of large scale production
- disadvantage:
- formation of anti nucleic acid antibodies possible
- integration of host vaccine DNA into host genome
- concept restricted to peptide and protein antigens
Vector vaccine
- vaccine introduced by vector
- vaccinia virus
Recombinant protein vaccine
- production involves insertion of DNA encoding an antigen such as a bacterial surface protein, which stimulates an immune response into bacterial or mammalian cells, expressing the antigen in these cells, and then the antigen is purified from them
- hepatitis B, HPV
Nucleic acid-based vaccine
- DNA plasmid/mRNA/recombinant vector
- contains viral genetic material (mRNA) which provides instructions for making viral proteins
- Zika
November 2019
SECTION A: TRUE AND FALSE QUESTIONS (20 MARKS)
STATE WHETHER THE FOLLOWING STATEMENTS ARE TRUE (T) OR FALSE (F).
1. Immune response is the first line of defense.
2. Adaptive defense system is consisting of an immune response.
3. Complement is the major innate mechanism that mediates destruction of foreign substances.
4. Regulatory T cells stimulate the proliferation of other lymphocytes.
5. Immunoglobulin G is the main antibody of both primary and secondary immune response.
6. Immunoglobulin E is involved in allergic reactions.
7. A graft from a monkey to a human is an example of an allograft.
8. Cellular ingestion and destruction of particulate matter are called phagocytosis.
9. Substances capable of triggering the adaptive immune system and provoking immune response are called antigen.
10. Tolerance for self-antigen is abnormal.
11. Autoimmune diseases are more common among men than women.
12. B and T cells can be distinguished from each other via a simple blood smear.
13. Major histocompatibility complex is associated with grafts rejection.
14. Anaphylaxis is an immediate hypersensitivity reaction.
15. A hapten when combined with a carrier can elicit the formation of antibodies.
16. Graft versus host disease is commonly associated with a corneal transplant.
17. Decreased capillary permeability can be seen in an inflammation process.
18. Immunoglobulin E is capable to fix complement.
19. Cellular antigens are involved in hypersensitivity type III.
20. B lymphocytes develop immunocompetence in the peripheral blood vessel.
SECTION B: SHORT ANSWER QUESTIONS (80 MARKS)
ANSWER ALL QUESTIONS
1. Describe hypersensitivity type I. (10 Marks)
IgE mediated
tissue injury caused by anaphylactic reaction
no complement involved
cells involved include mast cells, basophils, histamine granules
cytokines involved
ex of diseases include hay fever, asthma, food allergy
2. Describe common variable immunodeficiency. (10 Marks)
- defects in B cell differentiation into plasma cells
- complications: autoimmune disorder, lymphoid malignancy, bronchiectasis to recurrent pulmonary infections
- diagnosis: peripheral lymphadenopathy, family history, H/O recurrent infections
- lab: low IgG, IgA, IgM, antibody titer (against DPT/MMR vaccines)
- treatment: IVIG, immunosuppressant, antibiotics (chronic lung infections)
3. Explain the effects and mechanism of autoimmunity. (10 Marks)
4. Summarize the ideal vaccine for human. (10 Marks)
- safety: no ds cause by itself
- protection: prevent ds
- long lasting effects: induce T and B cell memory
- cost: inexpensive to produce and deliver
- administration: easy to deliver, no side effects
5. List the factors influencing tolerance and its’ application. (10 Marks)
- stage of differentiation of lymphocytes at the time of antigen confrontation
- site of encounter
- nature of cells presenting antigenic epitopes
- number of lymphocytes able to respond
- microenvironment of encounter
6. Describe mixed lymphocyte reaction test in tissue transplantation preparation. (10 Marks)
7. Explain alpha-fetoprotein (AFP) and carcino-embryonic antigen (CEA). (10 Marks)
8. Explain the mechanism for hypersensitivity type III. (10 Marks)
Ag-Ab immune complexes
immune complexes deposit on vessel wall
complement and neutrophil activation
release of pro-inflammatory cytokines, enzymes, reactive oxygen species
increased vessel permeability allows inflammatory molecules to cause tissue damage
ex of diseases include serum sickness, Arthus reaction
https://microbeonline.com/hypersensitivity-type-iii/
April 2019
SECTION B : SHORT ANSWER QUESTIONS (40 MARKS)
ANSWER ALL QUESTIONS.
Answer ALL questions by writing T for TRUE statement and F for FALSE statement in your answer booklet. (10 Marks)
1. Clonal deletion mechanism is activated after binding of MHC class to antigen-antibody-complement complexes.
2. Inflammation process starts with acute phase proteins which happen hours after tissue injury.
3. Binding of antigen-APC complex to TCR happen at secondary lymphoid organ.
4. T cells is proliferated from hematopoietic stem cells in bone marrow.
5. The secondary lymphoid organ is extremely deficient in trapping and concentrating foreign substance.
6. When antigen enter human body, it will be transported into spleen to interact with APC.
7. Interrelationship between innate immunity and acquired immunity is achieved by secretion of complements molecules.
8. Hapten is a high molecular weight substance which need to combine with other compounds to be immunogen.
9. MHC class II is activated when APC signals exogenous microbial infection.
10. Hypervariable region occurs only in light chain.
11. Variety of Ig classes is determined by heavy chain.
12. IgD involves in maturation of B cells after activation of MHC class I.
13. IgE is the major component in the colostrum. T
14. During the exponential state of antibody reaction, the increase and degradation of immunoglobulin happen at the balance rate.
15. IgM has higher avidity compared to IgG by 4 extra antigen-antibody binding sites.
16. T cytotoxic cells activation in adaptive immunity has memory.
17. Interaction of an immature B cell and self-antigen will reactivate mechanism of receptor editing.
18. Class switching involves IgM+IgD+B cells after the activation of CD4+ molecules to produces IgG, IgA or IgE molecules.
19. Humoral immunity is activated after production of MAC molecules through classical complement pathway and bindings to CD8+.
20. Cytokines like Tnf-alpha involve in response towards self-antigen which becoming non-self cell molecules.
2. By using appropriate diagram, describe the mechanism of how DNA vaccine works. (10 Marks)
3. Describe the principle of rapid test kit for dengue detection performed within the first three days after high fever. (10 Marks)
4. Describe the mechanism of acute graft rejection after transplantation. (10 Marks)
SECTION C: LONG ESSAY QUESTIONS (40 MARKS)
ANSWER ALL QUESTIONS.
Question 1
a. Describe the differences between hypersensitivity type II and III. (10 Marks)
T2H
- cytotoxic reaction
- antibody and cell-mediated
- antibody dependent, complement mediated
- IgG/IgM + cell bound antigen
- activate classical complement system
- opsonization and phagocytosis
- cytolysis
- ex: HDN
- ADCC
- Ag-Ab complex recognize by NK, macrophage, eosinophils, neutrophils with FcR
- release cytotoxic granules
- cause cell injury or death
- interference with cell function
- presence of antibody at receptor binding site
- impair cell function
- no inflammation, tissue damage
- activate: thyroid hormone receptor in Grave's disease
- inhibit: acetylcholine receptor in Myasthenia gravis
- disease: AIHA, hyperacute graft rejection, transfusion reactions
T3H
Ag-Ab immune complexes
- immune complexes deposit on vessel wall
- complement and neutrophil activation
- release of pro-inflammatory cytokines, enzymes, reactive oxygen species
- increased vessel permeability allows inflammatory molecules to cause tissue damage
- disease: serum sickness, Arthus reaction
https://microbeonline.com/hypersensitivity-type-iii/
b. Describe the differences between hypersensitivity type I and IV. (10 Marks)
T1H
- IgE mediated
- tissue injury caused by anaphylactic reaction
- no complement involved
- cells involved include mast cells, basophils, histamine granules
- cytokines involved
- disease: hay fever, asthma, food allergy, anaphylaxis
T4H
- delayed/cell-mediated
- disease: contact dermatitis, multiple sclerosis, chronic transplant rejection
b. Describe the immunofluorescent technique used to confirm diagnosis of Mycobacterium tuberculosis. (10 Marks)
September 2018
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Describe the differences between polyclonal and monoclonal antibody. (10 Marks)
polyclonal
- cheap
- heterozygous antibody population
- interact with different epitopes on same antigen
- produce by multiple clones of plasma B cells
- lot to lot variability
- increased likelihood of cross reactivity for similar antigens
monoclonal
- expensive
- homogenous antibody population
- interact with particular epitope
- produce by same clone of plasma B cells
- identical lots
- loss reactivity
2. a. Describe primary immunodeficiency caused by defective neutrophils. (5 Marks)
Chronic granulomatous disease
- genetic defects in NADPH
- which catalyzes reactive oxygen species
- ineffective phagocytosis
- increase infection susceptibility
- recurrent bacterial infections
- x linked or autosomal recessive
- treatment: IFN-𝛾
b. Describe type I hypersensitivity caused by paracetamol. (5 Marks)
allergen enters
antibody produced
at first, allergen is processed and presented by APC to CD4 T
activated CD4 T form Th and memory cell
Th produce IL4
at the same time B cell bind to antigen
IL4 activated
activated B form plasma cells and memory cells
plasma cells produce IgE
sensitization
IgE bind to mast cells and basophils
allergen enter 2nd time
antigen cross linked with Fab of IgE
degradation of mast cells and basophils
release pharmacological active chemicals (cytokines, histamine, heparin, serotonin, prostaglandin)
active chemical mediators acts on surrounding tissue
allergy
anaphylactic reaction
3. a. List the factors which may leads to false negative result in mycobacterium tuberculosis test. (5 Marks)
b. List the diseases which utilize IgE as the diagnostic marker. (5 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
Explain the immune response towards different bacterial infection category by using schematic diagram. (20 Marks)
https://www.creative-diagnostics.com/Infection-Immunity.htm
Question 2
a) Explain the tolerance mechanism towards cell expressing own surface marker. (10 Marks)
Anergy
- functional unresponsiveness to self antigen
- B cells
- interaction with T cells
- first signal
- absence of second signal
- apoptosis
- T cells
- TCR bind to MHC peptide on APCs
- first signal
- no IL2
- interaction with costimulatory molecules presenting by APCs
- activation aborted
Receptor editing
- rearrange Ig variable H or L chain
- secondary rearrangement at upstream V region
- delete receptor specificity
- delete RAG-1 or RAG-2 genes
Deletion
- autoreactive B and T are eliminated
- negative selection
- apoptosis
- double positive T cells bind with high affinity antigen and MHC
- rapid deletion
- immature B bind to strong affinity to self antigen in BM
- deletion
Clonal ignorance
- not anergy, deletion, receptor editing
- coexist with antigen
- remain inactivate
- weak affinity for autoantigen
- low concentration of autoantigen
b) Explain the mechanism of graft-versus-host-disease (GVHD) due to incompatible HLA typing. (10 Marks)
- donor CD4 T recognize recipient MHC2 foreign
- activated donor CD4 T
- cytokine release
- recipient macrophage, CD4 recruitment
- exacerbate/worsen cytokine response
- donor CD8 T recognize recipient MHC1 foreign
- activated CD8 T
- Fas, perforin mediated cytotoxicity
- majority of cell destruction at CD8 T
Question 3
Explain the different types of enzyme-linked immunosorbent assays (ELISA) technology. (20 Marks)
February 2018
SECTION B : SHORT ANSWER QUESTIONS (30 MARKS)
ANSWER ALL QUESTIONS.
1. a. Draw and label immunoglobulin A structure. (5 Marks)
b. List down the diseases related to immunodeficiency B cells (5 Marks)
- X linked agammaglobulinemia
- selective IgA deficiency
- transient hypogammaglobulinemia of infancy
- common variable deficiency
- hyper IgM syndrome
2. Describe the differences between tolerance divisions. (10 Marks)
central
- early stage of lymphocytes development
- site for T: thymus
- site for B: BM
- clonal deletion
peripheral
- mature stage of lymphocytes
- site: everywhere in the body
- both T and B cells
- anergy, cell death, immune deviation
3. Answer ALL questions by writing T for TRUE statement and F for FALSE statement in your answer booklet. (10 Marks)
1. Human immunodeficiency virus (HIV) is safe from immune attack when hiding in macrophages.
2. Immune system helps eliminating cancer cells after the equilibrium phase.
3. Activation of naïve T cells after the recognition of tumor cells will promote clonal expansion of effector T cells.
4. Autograft is the tissue transfer from siblings to burn patients as soon as the compatibility test was proven matched.
5. Cross-matching is testing the SERUM of the recipient for antibodies against the donor antigens.
6. Congenital agranulocytosis is an acquired disease which demonstrated by recurrent bacterial infections.
7. Flow cytometry method is based on cell surface marker expressed on the studied cell membrane and binding of specific antibody to the antigen.
8. Primary serological testing includes precipitation method done to detect the IgG in suspected dengue infection patient.
9. Strength of antibody-antigen reaction can be evaluated by serial dilution.
10. Cross reactivity can easily happen between the bindings of antigen to monoclonal antibody.
SECTION C: ESSAY QUESTIONS (40 MARKS)
ANSWER TWO (2) QUESTIONS ONLY.
Question 1
a. Explain the mechanism of graft versus host disease. (10 Marks)
- donor CD4 T recognize recipient MHC2 foreign
- activated donor CD4 T
- cytokine release
- recipient macrophage, CD4 recruitment
- exacerbate/worsen cytokine response
- TNF𝛼 possible cause of metabolic wasting
- donor CD8 T recognize recipient MHC1 foreign
- activated CD8 T
- Fas, perforin mediated cytotoxicity
- majority of cell destruction at CD8 T
b. Describe the immunological response in pathogenesis of colon cancer by using schematic diagram.(10 Marks)
- presence of tumor cells and tumor antigens
- initiate release of "danger" signals (heat shock proteins, cytokines, uric acid)
- activation and maturation of DC
- present tumor antigens to CD8 and CD4 T
- clonal expansion of CD8 and CD4 T
- migration from lymph node
- subsequent T cell mediated destruction of tumor cells
Question 2
a. Describe the mechanism of how DNA vaccine works by using appropriate diagram. (10 Marks)
b. Explain the mechanism of HIV destroy CD4 T cells by using appropriate diagram. (10 Marks)
Question 3
a. Describe the differences between hypersensitivity type I and II. (10 Marks)
b. Describe the differences between hypersensitivity type III and IV. (10 Marks)
September 2017
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Answer ALL questions by writing T for TRUE statement and F for FALSE statement in your answer booklet. (10 Marks)
1. Clonal deletion mechanism is activated after binding of MHC class to antigen-antibody-complement complexes
2. Inflammation process starts with acute phase proteins which happen hours after tissue injury
3. Binding of antigen-APC complex to TCR happen at secondary lymphoid organ
4. The secondary lymphoid organ is extremely deficient in trapping and concentrating foreign substance
5. When antigen enter human body, it will be transported into spleen to be interact with APC
6. Interrelationship between innate immunity and acquired immunity is achieved by secretion of complements molecules
7. Hapten is a high molecular weight substance which served as excellent immunogen
8. Protein is a better immunogen compared to carbohydrates because its complexity
9. MHC class II is activated when APC signals exogenous microbial infection
10. Variety of Ig classes is determine by heavy chain
11. IgD involves in maturation of B cells after activation of MHC class I
12. Immunoglobulin (Ig) A has four J chain
13. IgG has excellent capacity in immobilizing various motile bacteria by clumping the flagella and cilia of the organisms
14. IgM is the major component in the colostrum F
15. During the exponential state of antibody reaction, concentration on antibody increase exponentially and degradation of the Ig happen at the balance rate
16. IgM has higher avidity compared to IgG by 4 extra antigen-antibody binding sites
17. Interaction of an immature B cell and self-antigen will reactivate mechanism of receptor editing
18. Class switching involves IgM+IgD+B cells after the activation of CD4+ molecules to produces IgG, IgA or IgE molecules
19. Humoral immunity is activated after production of MAC molecules through classical complement pathway and bindings to CD8+
20. Inflammation event is part of first line defense mechanism
2. a. What is herd immunity? (2 Marks)
b. Describe DNA vaccines. (4 Marks)
c. What makes a successful vaccine production? (4 Marks)
safety
protection
cost
administration
3. a. List the factors which produce false negative result in HIV test. (5 Marks)
b. List the diseases which utilize IgE as the diagnostic marker. (5 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
a) Describe avoidance techniques of parasites from host immunological attack. (10 Marks)
a) Explain immunological defense mechanisms towards Mycobacterium sp. infection. (10 Marks)
Question 2
a) Explain the tolerance mechanism towards cell expressing own surface marker. (10 Marks)
b) Explain the mechanism of graft-versus-host-disease (GVHD) due to incompatible HLA typing. (10 Marks)
Question 3
a) Describe the immunological response in pathogenesis of breast cancer by using schematic diagram. (10 Marks)
- presence of tumor cells and tumor antigens
- initiate release of "danger" signals (heat shock proteins, cytokines, uric acid)
- activation and maturation of DC
- present tumor antigens to CD8 and CD4 T
- clonal expansion of CD8 and CD4 T
- migration from lymph node
- subsequent T cell mediated destruction of tumor cells
b) Describe the differences between hypersensitivity type II and IV. (10 Marks)
September 2017 (Special Exam)
SECTION A: SHORT ANSWER QUESTIONS (60 MARKS)
Answer ALL questions.
1. a. List the characteristic of primary immunodeficiency disease. (5 Marks)
- inborn
- inherited
- genetic mutations
- susceptible to recurrent, severe infections
- treatment: HSCT or IVIG
b. Briefly describe graft-versus-host-disease. (5 Marks)
damage to host as a result of a systemic inflammatory reaction included by T lymphocytes present in the graft
risk factors:
- HLA mismatch
- female donor to male recipient
etiology:
- transfusion of non irradiated blood products
- liver transplantation
- allogenic HSCT
- small bowel transplantation
signs and symptoms:
- maculopapular rash
- jaundice
- hepatosplenomegaly
- bloody diarrhea
- dyspnea
diagnosis: biopsy (skin, liver)
treatment: immunosuppressant
2. Describe the differences between polyclonal and monoclonal antibody. (10 Marks)
3. a. List the factors which produce false negative result in HIV test. (5 Marks)
b. List the allergens which contribute to hypersensitivity type I. (5 Marks)
- pollen
- nuts (food)
- insect stings
- influenza virus
- streptococci
- metal (nickels)
4. Describe the differences between hypersensitivity type II and IV. (10 Marks)
5. a. Describe primary immunodeficiency caused by defective neutrophils. (5 Marks)
b. State the factors which contribute to failure in immune response towards parasites infection. (5 Marks)
climate conditions, behavioral traits, host sociality, population density, diet, habitat, age, sex, host immunocompetence, supplementary feeding, and animal translocations
6. a. Describe hypersensitivity type I. (5 Marks)
b. State the autoimmune diseases categorized in localized autoimmune. (5 Marks)
- HT
- Addison
- Multiple sclerosis
- Goodpasture syndrome
- Atrophic gastritis
- Juvenile DM
SECTION B: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
a) Describe how RhoGm serves as prevention method from Rh isoimmunization among Rh negative mothers. (10 Marks)
b) Describe the ‘protection’ mechanism of a fetus from maternal antibody during the pregnancy. (10 Marks)
Question 2
a) Draw and label an immunoglobulin M molecule. (10 Marks)
b) Describe the differences between primary and secondary immunodeficiency. (10 Marks)
PID
- inborn
- inherited
- less common
- genetic mutations
- susceptible to recurrent, severe infections
- treatment: HSCT or IVIG
SID
- more common
- environmental factors
- bacterial and virus infections
- treatment: immunosuppressive drugs
- complication/cause: cancer, malnutrition, HIV, immunosuppressant/chemotherapy side effects
Question 3
a) Describe the differences between organ specific and systemic autoimmune diseases. (10 Marks)
Organ specific
- localized
- target for autoimmune attack: self antigen of given organ
- damage: organ
- treatment: replacement of organ function
- ex: HT, Addison, Multiple sclerosis
Systemic
- non organ specific
- targets for autoimmune attack: widespread self antigens
- damage: blood vessels
- treatment: inhibit excessive activation of immune system
- ex: SLE, RA, Sjogren syndrome
b) Compare immune responses towards virus and bacteria infections. (10 Marks)
Virus
- innate immunity
- inhibit binding to host cells
- stimulate complement molecules
- production of interferons
- kills infected cells with NK thro MHC1
- opsonization
- production of antibody by stimulate MHC2
- neutralize infection by reduce viral population
- production of memory cells
- protection against subsequent infection
Bacteria
- recognize foreign
- antigen receptor binds antigen
- release of cytokine
- send signals
- effector cells attack pathogens
- phagocytosis
January 2017
SECTION B : SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Describe the differences between hypersensitivity type II and IV. (10 Marks)
2. a. Describe primary immunodeficiency caused by defective neutrophils. (5 Marks)
b. List down the requirements for immunogenicity of an antigen for it to be able to cause human diseases. (5 Marks)
3. a. Describe how human immunodeficiency virus (HIV) is able to avoid host immune response. (5 Marks)
- enter bloodstream
- binds to DC carrying CD4 T
- initiates antibody and CTL production
- window period: 1~6 months
- destroy CD4 T
- epitope mutation
- escape from neutralization
b. List the diseases which utilize IgE as the diagnostic marker. (5 Marks)
SECTION C: ESSAY QUESTIONS (20 MARKS)
Answer TWO (2) questions ONLY.
Question 1
Explain the time course of immune response towards Bordetella pertussis infection by using schematic diagram. (20 Marks)
Question 2
Explain the different types of ELISA technology. (20 Marks)
Question 3
Explain in detail the technology used in new generation of vaccine. (20 Marks)
Recombinant vector
Recombinant attenuated
DNA
Gene deleted
Inactivated proteins, peptide based
August 2016
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Summarize the classification of adaptive immunity in illustration form. (10 Marks)
2. a. Briefly describe attenuated vaccine. (5 Marks)
b. List down the types of immunoproliferative diseases. (5 Marks)
multiple myeloma
plasma cell dyscrasias
Waldenstrom's macroglobulinemia
Hodgkin
Non Hodgkin
light chain disease
3. a. List the characteristic of primary immunodeficiency disease. (5 Marks)
b. Briefly describe graft-versus-host-disease. (5 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
Microbial infection could be classified into numerous categories which affects the human body differently as well as triggering different immunological pathways.
a) Describe how parasites manage to avoid immunological response upon their invasion. (10 Marks)
- parasite hide away
- invade immune-privileged tissue
- CNS, eyes
- some parasitoids place eggs in fat body
- parasite invisible
- achieve by shielding surface components
- parasite change antigenic surface during course of infection
- escape from recognition
- parasite stores variant
- Plasmodium falciparum approx. 60
- parasite evade by epitope mutation
- parasite temporary become inactive
b) Explain immunological defense mechanisms towards intracellular bacterial infections by using a schematic diagram. (10 Marks)
Question 2
Autoimmune disease is a state where body producing antibodies against our own normal cells. Most of autoimmune disease is caused by genetic mutation.
a) Describe the contributing factors of autoimmune disease. (10 Marks)
- genetic susceptibility
- predisposing genes
- severity modifying genes
- disease suppressing genes
- female gender
- estrogen progesterone
- chromosome XX
- unknown
- random variables
- Ig collection
- TCR collection
- external factors
- infections
- drugs, chemical
- pollution
- UV
- diet
- stress
b) Describe the mechanism of tolerance . (10 Marks)
Question 3
Explain the principles, benefit and diagnostic testing which use the following technique.
a) Immunoprecipitation (10 Marks)
b) Immunodiffusion (10 Marks)
January 2016
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Describe the differences between polyclonal and monoclonal antibody. (10 Marks)
2. a. Describe briefly primary immunodeficiency caused by defective neutrophils. (5 Marks)
b. Describe briefly type I hypersensitivity caused by paracetamol. (5 Marks)
3. a. List the factors which causes adaptive immunity to fail in eliminating human immunodeficiency virus (HIV) infection. (5 Marks)
b. List the diseases which utilize immunoglobulin E as the diagnostic marker. (5 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
Explain the time course of immune response towards bacterial infection by using a schematic diagram. (20 Marks)
Question 2
Explain the different types of enzyme-linked immunosorbent assays (ELISA) technology. (20 Marks)
Question 3
Describe the immunological response in pathogenesis of colon cancer by using a schematic diagram. (20 Marks)
August 2015
SECTION B : SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. a. List down the requirements for immunogenicity of an antigen for it to be able to trigger immune response. (5 Marks)
b. List down the immune molecules involved in response towards Candida sp infection. (5 Marks)
2. a. List down the diseases caused by hypersensitivity type I reaction. (5 Marks)
- hay fever
- asthma
- food allergy (nuts)
- anaphylaxis
- drug allergies (penicillin)
b. Name the common infectious agent isolated from to the following immunodeficient diseases. (5 Marks)
i. B cells
encapsulated bacteria
ii. T helper cells
virus, fungi, bacteria
iii. T cytotoxic cells
virus, fungi, bacteria
iv. immunoglobulins
v. complementary cells
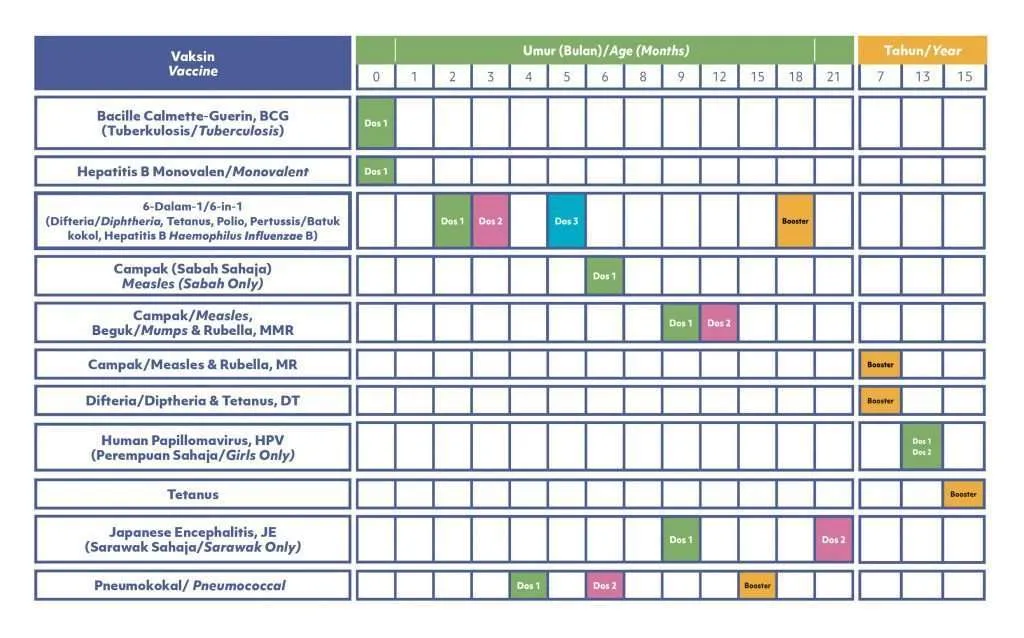
3. a. Recall the vaccination schedule in Malaysia. (8 Marks)
b. What are the advantages of using a vector vaccine? (2 Marks)
long lasting
stable gene transfer
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions ONLY.
Question 1
Bacterial infection could be classified into numerous categories which affects the human body differently.
1. Describe the immunogenic characteristics of bacteria in these various categories. (10 Marks)
2. Explain various immune defense mechanisms towards bacterial infections by using a schematic diagram. (10 Marks)
Question 2
Explain the principles, benefit and diagnostic testing which use the following technique.
1. immunoprecipitation (10 Marks)
2. agglutination. (10 Marks)
Question 3
Human immunodeficiency virus (HIV) positive is a retrovirus infection which causes acquired immunodeficiency syndrome (AIDS) and becomes a medical burden worldwide.
1. Describe how HIVs survive from human immune system recognition and attack. (10 Marks)
2. Describe the diagnostic techniques for HIV. (10 Marks)
ELISA
- detect HIV antibodies in blood
- sample of saliva or urine
- very sensitive
- false positive result
Western blot
Indirect FA
August 2014
SECTION B : SHORT ANSWER QUESTIONS (30 MARKS)
ANSWER ALL QUESTIONS
1. Describe the differences between type II and IV hypersensitivity. (10 Marks)
2. Describe the principles, benefits and differences between direct and indirect immunofluorescent technology. (10 Marks)
3. Describe the characteristics of attenuated vaccination. (10 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
ANSWER TWO (2) QUESTIONS ONLY
Question 1
Discuss the immunoediting mechanism in pathogenesis of Acute Lymphoid Leukemia. State also the immunological marker in Acute Lymphoid Leukemia diagnosis. (20 Marks)
Question 2
Explain ELISA and Western Blot test used in clinical setting. (20 Marks)
Question 3
Explain in detail the technology used in new generation of vaccine. (20 Marks)
January 2014
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions.
1. a. List FIVE (5) properties of ideal vaccines. (5 Marks)
- safety
- protection
- long lasting effects
- cost
- administration
b. Explain briefly about the attenuated vaccine. (5 Marks)
2. a. Define autoimmune diseases. . (2 Marks)
tissue injury
caused by humoral or cell-mediated
to self antigens
b. Describe FOUR (4) types of psoriasis. (4 Marks)
- plaque 80% (dry, scaling patches)
- nail 50% (dimpled)
- pustular rare (pus bumps)
- guttate 10% (hundreds of small scaly lesion)
c. List FOUR (4) laboratory diagnoses for insulin dependent diabetes mellitus. (4 Marks)
3. a. Name TWO (2) major oncofetal antigens in human. (2 Marks)
b. Explain each of your answer in (a). (8 Marks)
SECTION C: ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions only.
Question 1
Discuss the immunological basis of allergy in terms of (i) sensitization, (ii) mast cell activation, and (iii) late phase reaction. (20 Marks)
Question 2
Discuss the clinical progression and changes in the immune system during HIV infection. (20 Marks)
Question 3
Discuss in detail the types of enzyme-linked immunosorbent assay (ELISA). (20 Marks)
August 2013
SECTION B: SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions
1. Explain briefly the similarity and the differences between autoimmune organ specific and autoimmune non-organ specific diseases. (10 Marks)
2. Describe the required laboratory tests to diagnose each type of hypersensitivity. (10 Marks)
3. Describe the escape mechanism and immune surveillance in tumorigenesis. (10 Marks)
SECTION C: ESSAY QUESTIONS (20 MARKS)
Answer TWO (2) questions ONLY.
Question 1
ELISA method has been used widely to detect existence of protein. Explain in detail the protocol of indirect ELISA and compare it with direct ELISA. Support your answer with labeled diagram. (20 Marks)
Question 2
AIDS is an immunosuppressed disease caused by infection of Human Immunodeficiency Virus (HIV). Explain in detail the pathophysiology of the disease, immune response towards the viral infection, laboratory diagnosis that can be done to the suspected individual and factors that make HIV is hard to detect at the early phase. (20 Marks)
Question 3
Vaccination has been used for a very long time and successfully eliminated many fatal infectious diseases. Explain in detail the differences between passive and active vaccination. (20 Marks)
July 2011
PART B : SHORT ANSWER QUESTIONS (30 MARKS)
Answer ALL questions.
1. a. Differentiate between organ specific and systemic autoimmunity. (2 Marks)
b. Describe the autoimmunity associated with thyroid gland. (4 Marks)
c. Explain how the insulin-dependent diabetes mellitus patient (4 Marks) develop tissue injury and describe the appropriate treatments to control and cure the disease.
2. a. Define the term transplantation and give examples. (2 Marks)
transfer an organ or part of an organ from one donor to either themselves or other recipient or their identical recipient
b. Differentiate among four types of grafts. (4 Marks)
- auto (recipient's)
- iso (genetic identical)
- allo (genetic different)
- xeno (other species)
c. Predict the mechanism of graft rejection and symptoms (4 Marks) developed when an immunocompromised patient received a skin graft from normal individual.
3. a. List and explain the etiology of tumor. (4 Marks)
- inherited
- chemical (carcinogen)
- viral (HPV)
- radiological (UV)
- abnormal cell growth (fail in control)
b. Describe the factors that can cause transformation of normal (2 Marks) cells into malignant cells.
c. Demonstrate how the components of immune system (4 Marks) response against tumor associated antigens.
PART C : ESSAY QUESTIONS (40 MARKS)
Answer TWO (2) questions only.
Question 1
Differentiate between extracellular and intracellular bacteria. Explain how the bacteria can cause diseases in human and describe the immunity against the infections caused by both bacteria. (20 Marks)
Question 2
Determine two types of vaccines which are safe to be administered to the AIDS’s patient. Describe how the vaccines can be developed and state the advantages and disadvantages of using the vaccines. (20 Marks)
Question 3
Describe the classification of immunodeficiency disorder. Demonstrate how immunodeficiency can lead to infections in patient with severe combined immunodeficiency (SCID) and individuals with acquired immune deficiency syndrome (AIDS). (20 Marks)
PID
SID
SCID
- defects in stem cell maturation
- adenosine deaminase deficiency
- manifestation (3 months): recurrent severe bacterial, viral, fungal, protozoan infections, failure to thrive, diarrhea, dermatitis, candida
- lymphopenia, low IgA, IgG, IgM
- treatment: isolation, treat underlying infections, BM transplant
AIDS
January 2010
PART B (25 MARKS)
Answer ALL questions.
1. An outbreak of a flu-like illness has occurred in your student housing complex. The doctor on-call at the university medical center suspects that the outbreak is due to the SARS virus because one of the students living in the housing complex had recently returned from a research trip to animal markets in Guan Dong, China. You, the MLT working in the medical center, have been asked to perform an ELISA to confirm the doctor’s suspicions.
In your laboratory you have available the following materials and reagents.
Anti-SARS-CoV antibody from mouse
Anti-mouse immunoglobulin antibody conjugated to HRP
Enzyme substrate for HRP (TMB)
Wash buffer
a. Identify the following components that you would need to perform an ELISA to detect the SARS virus (SARS-CoV antigen) in the students’ serum samples.
COMPONENT
Material Required
Antigen to be tested
Student’s serum samples
Primary Antibody
Secondary Antibody
Positive Control
Heat-inactivated SARS-CoV antigen
Negative Control
(3 marks)
b. Using the materials you have available to you as above, describe the steps to perform an ELISA to detect the presence of the SARS-CoV antigen in the student’s serum samples. (15 marks)
c. What would you expect to observe in the test microplate well if the student’s sample was:
v. positive for SARS-CoV antigen? (1 mark)
vi. negative for SARS-CoV antigen? (1 mark)
d. The ELISA to detect the SARS-CoV antigen can also be modified to make it quantitative (i.e. to calculate the amount of antigen present in the student’s serum sample. What principle will enable you to do this? (3 marks)
e. What does ELISA stand for? (1 mark)
enzyme linked immunosorbent assay
f. Give one other antigen you can detect in serum using ELISA. (1 mark)
hepatitis
PART C (45 MARKS)
Answer any THREE (3) questions.
1. Compare and contrast attenuated vaccines & inactivated vaccines. (15 marks)
2. Explain how graft versus host disease can develop after bone marrow transplantation. (15 marks)
3. Explain how you would perform the tuberculin skin test on an allergy patient. How would you interpret the results? (15 marks)
4. Describe the immune mechanisms involved in the development of hemolytic disease of the newborn. (15 marks)















Comments
Post a Comment